World COPD Day … Interpretation of GOLD 2021 Guidelines on novel coronavirus pneumonia and chronic obstructive pulmonary disease
The Global Initiative for Chronic Obstructive Pulmonary Disease (COPD) (GOLD) has just released the 2021 Global Strategy for the Diagnosis, Treatment and Prevention of Chronic Obstructive Pulmonary Disease (GOLD 2021). Different from previous years' GOLD guidelines, GOLD 2021 focuses on the relationship between COVID-19 pneumonia and COPD in the context of the COVID-19 epidemic, providing a reference scheme for doctors around the world to deal with the complex relationship between COPD patients and COVID-19 pneumonia. This article describes the highlights of this section of the Guide.
I. Introduction
The widespread spread of severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2), which led to the global COVID-19 outbreak, has greatly troubled the diagnosis and treatment of patients with COPD. Based on the results of numerous studies published by clinical researchers worldwide on COVID-19, this chapter provides a relatively complete and provisional guide to the relationship between COVID-19 and COPD and the management of their combination.
2. Risk of SARS-CoV-2 infection in COPD patients
At present, there is no clear evidence that COPD increases the risk of SARS-CoV-2 infection. However, coexisting COPD increases the risk of hospitalization in COVID-19 patients (HR 1.55; 95%CI 1.46-1.64). Some studies suggest that COPD will increase the proportion of COVID-19 patients developing severe disease and increase the case fatality rate, which may be caused by poor compliance, difficulties in self-management, difficulties in seeking medical treatment during the epidemic, and decreased lung function reserve. Studies have also reported that smoking leads to the aggravation of COVID-19 and increased mortality, and smoking is closely related to the occurrence and development of COPD.
3. Relevant laboratory inspection
1, SARS-CoV-2 infection detection
Patients with COPD who develop respiratory symptoms, fever, and other COVID-19-related symptoms, even if the symptoms are mild, should be tested for SARS-CoV-2 nucleic acid PCR for infection. At the same time, SARS-CoV-2 test results cannot exclude the possibility of infection by other pathogens. There have been cases reported of viral reactivation or viral reactivation in COVID-19 patients, so retesting is needed if necessary.
2. Spirometry and pulmonary function test
Spirometry and pulmonary function tests themselves may cause SARS-CoV-2 virus transmission, which may be caused by the formation of droplets caused by coughing during the examination. Therefore, during the COVID-19 epidemic, these tests need to be strictly limited and only performed when necessary. At the same time, if routine pulmonary function tests are limited, home peak expiratory flow rate (PEF) measurements and accurate questionnaires can also help in the diagnosis of COPD.
3. Tracheoscope
If a patient with COPD needs a tracheoscopy during an epidemic, a negative nucleic acid result is necessary. In case of emergency, adequate protection is required.
4. Imaging examination
For mild or asymptomatic infected persons, the sensitivity of chest radiography is poor. For general and severe patients, chest radiograph can help to determine the change of disease. The value of chest CT is well established and has been used for the diagnosis of COVID-19 and the determination of disease severity, which is no different in patients with COPD. Due to the increasing number of cases reported in COVID-19 patients complicated with deep vein thrombosis and pulmonary embolism, timely CT examination is needed if pulmonary embolism is considered.
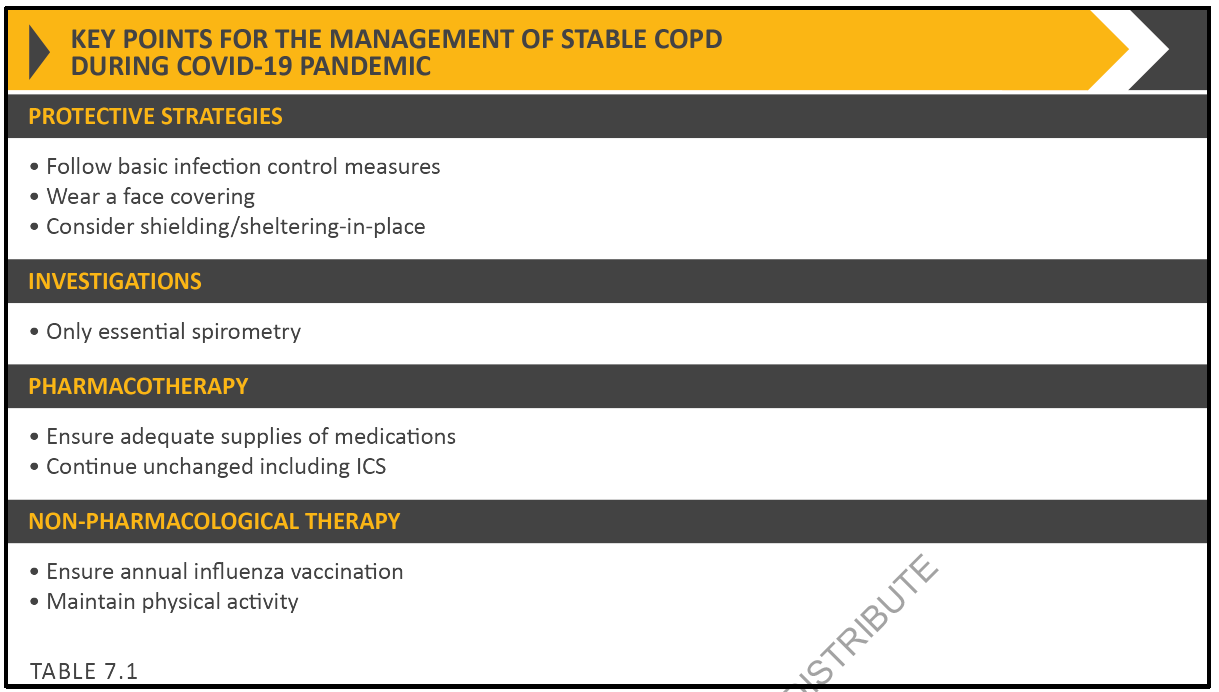
Iv. Key points of stable COPD disease management during the COVID-19 epidemic
1. Protective measures: Observe basic infection prevention and control measures, wear masks, and reduce personal contact and exposure.
2, check: If not necessary, not vital capacity test.
3, drug treatment: ensure adequate drug supply; Do not change the usual inhaled hormone therapy.
4, non-drug treatment: flu vaccine; Proper body function exercise.
5. Distinguish daily symptoms of COPD from COVID-19 infection
It is challenging to distinguish the symptoms of COVID-19 infection from the everyday symptoms of COPD patients. Most COVID-19 patients may have a dry cough, shortness of breath, and more than 60% May be accompanied by fever, while fatigue, disturbance of consciousness, diarrhea, nausea, vomiting, muscle aches, smell disorders, taste disorders, headaches, etc.
If COPD patients have early mild prodromal symptoms, they may be ignored, affecting early diagnosis. Even when symptoms worsen and COVID-19 is suspected, repeated testing is rare. Patients with COPD should be alert to COVID-19 when their daily symptoms worsen, especially when accompanied by fever, taste and smell disorders, or gastrointestinal symptoms.
Diagnosing COVID-19 is difficult in COPD patients with persistent respiratory symptoms. Only 65% of SARS-CoV-2-positive COPD patients returned to their previous state of health after 2-3 weeks. Some patients have coughing, fatigue and shortness of breath for weeks, and in a few cases for months. Delayed recovery is more common in patients with multiple chronic diseases, including COPD.
6. Maintenance of COPD medication during the COVID-19 epidemic
There are concerns that inhaled corticosteroids (ICS) may increase the risk of infection in COPD patients. At present, studies have suggested that ICS may reduce the replication of coronavirus-including SARS-CoV-2, and may have a protective effect on the body's resistance to COVID-19, but it has not been confirmed by clinical studies. To date, there is no clear evidence that changing COPD medication reduces the prevalence of COVID-19, nor is there evidence to support that maintaining ICS inhalation increases the risk of COVID-19 infection. Therefore, patients with COPD are advised to continue their usual drug therapy during the COVID-19 epidemic.
Because atomization increases the transmission of SARS-CoV-2 and increases the risk of infection, pressure dose inhalers, dry powder inhalers, and soft mist inhalers are recommended to replace atomization therapy if conditions permit. Once atomization is necessary, it is necessary to avoid the spread of disease as much as possible, such as avoiding the presence of others, close to the window, etc.
7. Maintain non-drug treatment for COPD during the COVID-19 epidemic
Non-drug treatments, including flu shots, appropriate limb exercises, and palliative care, are an important part of the treatment strategy for COPD patients. During COVID-19, patients with COPD need to maintain their non-drug treatment strategies. There is no evidence to support changes in palliative care for COPD patients due to COVID-19.
8. Treatment of COPD combined with COVID-19
1. Systemic hormone application
At the early stage of the epidemic, WHO did not recommend systemic hormone therapy for COVID-19 patients, except for two cases, ARDS and acute exacerbation of COPD. At present, several studies have suggested that systemic use of hormones may improve COVID-19 outcomes in certain patients. At present, there is no evidence to prove that hormones increase the risk of COVID-19 in COPD patients, and there is no evidence to support that systemic use of hormones will worsen the condition of acute exacerbations of COPD. Therefore, systemic glucocorticoids should be routinely used in patients with acute exacerbations of COPD, regardless of whether COVID-19 is present.
2. Antibiotics
Current WHO guidelines recommend the use of broad-spectrum antibiotics in patients with severe COVID-19 and antibiotics in patients with mild COVID-19 if bacterial infection is clinically suspected. These principles should also be followed in patients with COPD combined with COVID-19.
Antibiotics should be used in patients with acute exacerbations of COPD, with or without COVID-19.
3. Mechanical ventilation
Noninvasive positive pressure ventilation is the standard treatment for COPD patients with acute respiratory failure. In COPD patients with hypercapnia associated with COVID-19 pneumonia, the use of non-invasive positive pressure ventilation may benefit, but may also increase the risk of lung injury due to transpulmonary pressure and tidal volume. At the same time, for patients with COPD combined with COVID-19 pneumonia who need respiratory support, whether using nasal high flow or non-invasive positive pressure ventilation, the condition changes should be closely monitored, and invasive mechanical ventilation should be performed with tracheal intubation if necessary. Oxygenation index less than 150mmHg may be used as an indicator of non-invasive positive pressure ventilation failure and high mortality. It is important to note that medical personnel must adopt perfect personal protection during mechanical ventilation, and mechanical ventilation equipment should also use a suitable virus filtration system.
4. Rehabilitation and follow-up
For patients with COPD combined with COVID-19, early recovery is necessary. The above patients also need to be closely followed up after discharge, including early and long-term follow-up, and there are corresponding procedures.
9. Summary of key points
That is an overview of Chapter 7 of the guide. To sum up the following points:
1. In COPD patients with new or worsening respiratory symptoms, fever, and other symptoms that may indicate COVID-19, it is recommended to improve SARS-CoV-2 nucleic acid testing, even if the symptoms are mild.
2. During the COVID-19 epidemic, there is no evidence to support changes in oral and inhaled medication for patients with COPD.
3. In communities at high risk of COVID-19, testing of vital capacity and lung function needs to be severely limited.
4, physical distance does not increase social barriers between people, COPD patients can keep in touch with relatives and friends through the phone or the Internet, at the same time, to ensure that there is enough medicine.
5. Encourage patients to access medical knowledge about COVID-19 through trusted information channels.
6. Follow-up of patients with COPD can be conducted in a variety of ways, including telephone and Internet.

